Guidelines for the Treatment of Adults with Metastatic Brain Tumors
5. The Role of Chemotherapy in the Management of Adults with Newly Diagnosed Metastatic Brain Tumors
Download PDF Neurosurgery, 2019
Sponsored by: The Congress of Neurological Surgeons and the Section on Tumors
Affirmation of Educational Benefit by: The Congress of Neurological Surgeons and the American Association of Neurological Surgeons
Jonathan H. Sherman, MD,1 Simon S. Lo, MD,2 Tom Harrod, MS, MLS,3 Alia Hdeib, MD,4 Yiping Li, MD,5 Timothy Ryken, MD, MS6 and Jeffrey J. Olson, MD 7
- Department of Neurosurgery, The George Washington University, School of Medicine and Health Sciences, Washington, DC, USA
- Department of Radiation Oncology, University of Washington School of Medicine, Seattle, Washington, USA
- Himmelfarb Health Sciences Library, The George Washington University, School of Medicine and Health Sciences, Washington, DC, USA
- Department of Neurological Surgery, Case Western Reserve University, Cleveland, Ohio, USA
- Department of Neurosurgery, University of Wisconsin, Madison, Wisconsin, USA
- Section of Neurosurgery, Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire, USA
- Department of Neurosurgery, Emory University, Atlanta, Georgia, USA
Correspondence:
Jonathan H. Sherman, MD
Department of Neurosurgery
George Washington University Medical Center
2150 Pennsylvania Avenue, NW Suite 7-408
Washington, DC 20037, USA
Email: jsherman0620@gmail.com
All authors contributed equally to this work.
Disclaimer of Liability
This clinical systematic review and evidence-based guideline was developed by a multidisciplinary physician volunteer task force and serves as an educational tool designed to provide an accurate review of the subject matter covered. These guidelines are disseminated with the understanding that the recommendations by the authors and consultants who have collaborated in their development are not meant to replace the individualized care and treatment advice from a patient's physician(s). If medical advice or assistance is required, the services of a competent physician should be sought. The proposals contained in these guidelines may not be suitable for use in all circumstances. The choice to implement any particular recommendation contained in these guidelines must be made by a managing physician in light of the situation in each particular patient and on the basis of existing resources.
Keywords:
Brain metastases, cerebral metastases, chemotherapy, practice guideline, stereotactic radiosurgery, systematic review, whole brain radiation therapy
ABSTRACT
Question 1: Should patients with brain metastases receive chemotherapy in addition to whole brain radiation therapy (WBRT) for the treatment of their brain metastases?
Target population: This recommendation applies to adult patients with newly diagnosed brain metastases amenable to both chemotherapy and radiation treatment.
Recommendations
Level 1: Routine use of chemotherapy following WBRT for brain metastases is not recommended.
Level 3: Routine use of WBRT plus temozolomide is recommended as a treatment for patients with triple negative breast cancer.
Question 2: Should patients with brain metastases receive chemotherapy in addition to stereotactic radiosurgery (SRS) for the treatment of their brain metastases?
Recommendations
Level 1: Routine use of chemotherapy following SRS is not recommended.
Level 2 : SRS is recommended in combination with chemotherapy to improve overall survival and progression free survival in lung adenocarcinoma patients.
Question 3: Should patients with brain metastases receive chemotherapy alone?
Recommendation
Level 1: Routine use of cytotoxic chemotherapy alone for brain metastases is not recommended as it has not been shown to increase overall survival.
INTRODUCTION
Rationale
Brain metastases commonly present in patients with systemic malignancy. As systemic treatment has improved, and patients are displaying an increase in overall survival, the incidence of brain metastases has also increased, ranging between 20 and 40%.1, 2 Traditional cytotoxic chemotherapeutics have been proven to provide limited efficacy to intracranial pathology, secondary to their inability to cross the blood-brain barrier (BBB). The increase in the incidence of brain metastases with new chemotherapeutics corresponds with this finding. Despite disruption of the BBB with the growth of these tumors, they do not appear to receive a cytotoxic level of the drugs.3 There are limited data regarding the response of certain cancer subtypes to a higher degree with regard to brain metastases. These include subtypes of breast carcinoma and lung carcinoma among others. In an effort to circumvent the issue presented by the BBB, new treatment strategies are being developed that can treat both the primary and metastatic systemic malignancy as well as the metastatic intracranial malignancy. These treatment modalities include such areas as targeted agents to key receptors involved with tumor progression (ie, epidermal growth factor receptor, HER-2) and immunotherapy. Despite these promising new treatment options, the mainstay of treatment for brain metastases is radiation therapy. There exists a growing body of literature discussing the increasing efficacy of stereotactic radiosurgery (SRS) and delaying whole brain radiation therapy (WBRT).4
Objectives
No definitive trial has established a routine role for chemotherapy for the treatment of brain metastasis, either as stand-alone treatment for brain metastases or in combination. This literature review sought to identify evidence-based guidelines for the use of chemotherapy as a stand-alone treatment for brain metastases or in combination with either WBRT or SRS. This review serves as an update to the review by Mehta et al. 2010 2. In the original review, the primary question involved the efficacy of WBRT used in addition to chemotherapy based on literature from 1990 to September 2008. The current review looked at literature published since the prior report to answer this question. In addition, the authors sought to address the efficacy of chemotherapy in addition to SRS, as well as the role of chemotherapy as a stand-alone treatment. In an effort to address these 3 questions, the authors identified 8 primary categories in the published literature:
1. Chemotherapy vs chemotherapy + WBRT
2. WBRT vs WBRT + chemotherapy
3. Chemotherapy first, followed by WBRT vs WBRT first, followed by chemotherapy
4. Sequential or concomitant chemotherapy + WBRT
5. WBRT + 2 concurrent chemotherapeutic regimens
6. Chemotherapy vs chemotherapy + WBRT vs chemotherapy + SRS
7. Chemotherapy + WBRT vs chemotherapy + WBRT + SRS
8. Chemotherapy vs chemotherapy + SRS
METHODS
Search Strategy
To answer the questions stated above, a comprehensive systematic review of the literature was performed. The following electronic databases were searched from 1990 to December 31, 2015: MEDLINE, Cochrane Database of Systematic Reviews, Cochrane Controlled Trials Registry, and Cochrane Database of Abstracts of Reviews of Effects. A broad search strategy using a combination of subheadings and text words was employed. The bibliography of included studies were also reviewed.
For inclusion in this analysis, the following criteria had to be met:
• Published in English with a publication date of 1990 forward for the SRS search.
• Published in English with a publication date of 2008 forward for the WBRT search.
• Patients with newly diagnosed brain metastases.
• Fully published peer-reviewed primary comparative studies (all comparative study designs for primary data collection included; eg, RCT, non-randomized trials, cohort studies or case-control studies).
• Any comparative studies evaluating chemotherapy alone or in combination with other treatment modalities for the treatment of newly diagnosed brain metastases.
• Number of study participants with newly diagnosed brain metastases > or = 5 per study arm for at least two of the study arms.
Study Selection and Quality Assessment
Studies that met the eligibility criteria had their data extracted by one reviewer, and the extracted information was checked by a second reviewer.
Evidence Classification and Recommendation Levels
Both the quality of the evidence and the strength of the recommendations were graded according to the American Association of Neurological Surgeons (AANS)/Congress of Neurological Surgeons (CNS) criteria. These criteria are provided in the methodology paper for this guideline series and can also be found at here
Guideline Development Process
The Joint Tumor Section of the AANS/CNS convened a multi-disciplinary panel of clinical experts to develop a series of evidence-based practice guidelines on the management of brain metastases based on a systematic review of the literature conducted in collaboration with the CNS Guidelines Office and local university reference librarians.
Risk of Bias across Studies
Bias was assessed across all studies. The primary form of bias involved the assessment of selective reporting across studies.
RESULTS
The literature search resulted in the identification of 3,170 citations, of which 3,146 were eliminated at abstract review as not having relevance to the specific questions. The remaining 24 studies were subject to full-text screening, and 7 were excluded because the data were heavily weighted toward targeted agents and not cytotoxic chemotherapeutics. Seventeen eligible studies5-21 were therefore fully reviewed and form the basis for this report (see Tables 1-3; Figure 1).
These 17 studies were assigned to the eight primary categories above as follows:
1. Chemotherapy vs chemotherapy + WBRT: 4 studies.13-15, 21
2. WBRT vs WBRT + chemotherapy: 7 studies.5-7, 11, 12, 17, 20
3. Chemotherapy first, followed by WBRT vs WBRT first, followed by chemotherapy: 1 study.9
4. Sequential or concomitant chemotherapy + WBRT: 1 study.19
5. WBRT + 2 concurrent chemotherapeutic regimens: 1 study.16
6. Chemotherapy vs chemotherapy + WBRT vs chemotherapy + SRS: 1 study. 8
7. WBRT + SRS vs Chemotherapy + WBRT + SRS vs TT + WBRT + SRS: 1 study. 18
8. Chemotherapy vs chemotherapy + SRS: 1 study.10
Through this exhaustive search of the literature, it is readily apparent that a limited number of randomized controlled trials have been performed that address this topic of interest. Consequently, the overall applicability of the recommendations generated from this search is limited. The original guidelines that were published in 20102 only addressed the efficacy of chemotherapy in combination with WBRT. Interestingly, the number of studies addressing this same question since the original guidelines were developed is far greater than those involving SRS specifically for cytotoxic chemotherapy. The majority of studies that combined SRS with a therapeutic agent involved either a targeted agent or an immunotherapy drug and was eliminated for evaluation in this manuscript. These studies are addressed in a manuscript specifically looking at emerging therapies for patients with brain metastases (please refer to Tables 1-3 for details of the included studies). A combination of these 8 categories were used to answer the 3 primary questions such that articles fitting categories 1- 5 were used to address the efficacy of WBRT, articles fitting categories 6-8 were used to address the efficacy of SRS, and categories 1 and 6 were used to address the efficacy of chemotherapy alone.
Should patients with brain metastases receive chemotherapy in addition to whole brain radiation therapy (WBRT)?
(1) Chemotherapy vs chemotherapy + WBRT
Four studies13-15, 21 met the inclusion criteria for this category. Three of the 4 studies provided Class I evidence (phase III randomized controlled trials), and the fourth was a retrospective cohort study, and provided Class II evidence.
Neuhaus et al.21 performed a phase III randomized controlled trial in 2009 studying the role of chemotherapy plus WBRT (G1) versus chemotherapy alone (G2) in patients with lung metastases. The authors evaluated 96 adult patients with both small cell lung carcinoma (SCLC) and nonSCLC (NSCLC). The patients received WBRT at a dose of 2 Gy per treatment for a total of 40 Gy. The chemotherapeutic drug was topotecan given at a dose of 0.4 mg/m2/day for 5 days over 4 weeks and 2 hours prior to WBRT. The G1 group enrolled 47 patients and the G2 group enrolled 49 patients. The non-hematologic toxicities were evenly distributed among groups. With regard to hematologic events, 24 occurred in the G1 group and 1 occurred in the G2 group. Neither OS (p = .43) nor PFS (p = .89) differed significantly between groups. This was true for both the SCLC and NSCLC cohort. These results and an overall slow recruitment resulted in termination of the study following interim analysis.
Mornex et al.13 published the results of a prospective randomized phase III trial in 2003 comparing fotemustine plus WBRT (n = 37) and fotemustine alone (n = 39) in patients with cerebral metastases from malignant melanoma. The main objectives were objective response and time to brain progression. Patients with histologically confirmed malignant melanoma with at least one non-resectable metastasis and who fit other parameters were included. It was required that patients had received no chemotherapy in the prior 4 weeks, no previous nitrosourea-based chemotherapy, and no previous brain radiotherapy. Both arms were well balanced with regard to the number of brain metastases, extent of visceral disease, and age. Patients in the fotemustine alone arm had worse baseline performance status (ECOG 2-3 54% compared with 30% in the fotemustine plus WBRT arm) and had been treated with more chemoimmunotherapy in a higher proportion (59% vs 32% respectively). Furthermore, the median time intervals between the primary diagnosis and the onset of brain metastases were different between the two arms (550 days for the fotemustine alone arm vs 1131 days for the fotemustine + WBRT arm). The prescribed dose of WBRT was 37.5 Gy in 15 fractions over 3 weeks. Fotemustine was given intravenously at 100 mg/m2 on days 1, 8, and 15, followed by a 5-week rest period, and then every 3 weeks in non-progressing patients. Although the patients who had fotemustine alone had worse prognostic factors, there was no difference in brain response or local control or in overall survival (86 days in the fotemustine arm vs 105 days in the combined modality arm). There was a statistically significant difference in the time interval to brain progression, favoring the WBRT + fotemustine group (p = .028) (median time to objective brain progression of 56 days compared with 49 days in the chemotherapy alone arm).
Postmus et al15 reported the results of a phase III randomized study in 2000 comparing teniposide (arm 1) versus teniposide with WBRT (arm 2) in patients with brain metastases from SCLC. The stated aim of the trial was to evaluate the role of WBRT in SCLC patients with brain metastases. The primary end point was survival. Teniposide was administered intravenously at 120 mg/m2 on days 1, 3, and 5 every 3 weeks up to a maximum of 12 courses, or until disease progression either intra- or extra-cranially. WBRT, delivering 30 Gy in 10 fractions over 2 weeks, had to be started within 3 weeks of the start of treatment with teniposide. Dexamethasone dosing parameters were outlined. Among the 134 patients randomized, 120 were eligible with 60 in each group. The groups were well matched for age, ECOG performance status, neurologic function, and number of brain metastases. Despite the higher response rate of 57% (vs 22%) in the combined modality group (arm 2) compared to the teniposide alone group (arm 1), this did not translate into a prolongation of overall survival. This was thought to be due to progression of disease outside the brain (3.2 months in Arm1 and 3.5 months in arm 2). Time to progression in the brain was evaluated using CT scan instead of MRI in this European study and was significantly longer in the combined modality group.
In a retrospective cohort study by Moscetti et al14 in 2007, 110 patients (cohort 1) with newly diagnosed NSCLC with brain metastases receiving upfront platinum-based chemotherapy were compared with 46 patients who receiving WBRT followed by chemotherapy (cohort 2). The investigators attempted to analyze the process by which six oncology centers guided the pattern of care. In this survey of unselected patients, the choice of treatment appeared to be guided by presence of neurologic symptoms from the brain metastases. The response rate in the brain was 27.3% in cohort 1 and 34.8% in cohort 2 with no significant difference in median time to progression in the brain (6 months for both cohorts). With regard to the first treatment option, the median survival was 10 months for cohort 1 and 14 months for cohort 2.
Risk of bias across studies
In the Postmus et al.15 study, time to progression in the brain was evaluated using CT scan instead of MRI which may generate bias. Although the study by Moscetti et al. 14 showed that some patients with brain metastases from NSCLC will respond initially to platinum-based chemotherapy, there were too many confounding factors that hamper unbiased evaluation, rendering it very difficult to derive any meaningful data for recommendation.
(2) WBRT vs WBRT + chemotherapy
Seven studies5-7, 11, 12, 17, 20 met the inclusion criteria for this category. Five of the 7 studies provided Class I evidence (three are phase II randomized controlled trials and two are meta-analyses). Two studies provided Class II evidence (one is a prospective cohort study and one is a non-randomized phase II controlled trial). Cao et al.5 performed a phase II randomized controlled trial in 2015 studying the role of WBRT alone (G1) versus chemotherapy plus WBRT (G2) in patients with breast carcinoma. The authors evaluated 100 adult patients. WBRT was provided at a dose of 3 Gy in 10 fractions for a total of 30 Gy. The chemotherapeutic drug was temozolomide at a dose of 75 mg/m2/day for a total of 14 days. Each group initially enrolled 50 patients. Of the patients, 40 displayed ER, PR positive and Her-2 negative, 33 specimens displayed ER, PR, and Her-2 negative, and 19 specimens displayed HER-2 positive. For final endpoint analysis, the G1 group had 47 patients and the G2 group had 37 patients.
The relative response rate was 36% in the G1 group and 30% in the G2 group. The median overall survival (OS) was 11.1 months in the G1 group and 9.4 months in the G2 group. The median progression-free survival (PFS) was 7.4 months in the G1 group and 6.8 months in the G2 group. For patients with HER2 positive tumors, the OS was 16.1 months in the G1 group and 20.2 months in the G2 group. The PFS was 15 months in the G1 group and 13.1 months in the G2 group. For patients with ER, PR positive, Her-2 negative tumors, the OS was 9.3 months in the G1 group and 9.4 months in the G2 group. The PFS was 6.7 months in the G1 group and 5.1 months in the G2 group. In patients with triple negative tumors, the OS was 4.9 months in the G1 group and 9.2 months in the G2 group. The PFS was 2.8 months in the G1 group and 8.0 months in the G2 group. Overall, there was no significant difference in either OS or PFS between groups. While the power was too small for statistical analysis for the subgroups, the patients with triple negative tumors displayed a noticeable difference in both OS and PFS after receiving temozolomide plus WBRT as compared to the patients receiving WBRT alone.
Chua et al.6 performed a phase II randomized open-label trial in 2010 studying the role of chemotherapy plus WBRT (G1) versus placebo plus WBRT (G2) in patients with brain metastases from NSCLC. The study enrolled 95 patients from 35 sites in 14 countries. The KPS was > or = 70 in all patients. The patients received WBRT with a total of 30 Gy given in 10 fractions over 2 weeks. Temozolomide was given as the chemotherapeutic drug at a dose of 75 mg/m2 for 21 days in group G1 versus placebo in group G2.
Systemic disease was stable in 52% of patients at the time of enrollment. More patients in the G1 group had brain metastases at presentation as compared to the G2 group (30% vs 13%) (p < .47). In addition, more patients in the G1 group received prior chemotherapy as compared to the G2 group (81% versus 51%) (p < .025). Treatment compliance was 91% in the G1 group and 96% in the G2 group. Median OS was 4.4 months in the G1 group and 5.7 months in the G2 group (p = .59). Median CNS PFS was 3.1 months in the G1 group and 3.8 months in the G2 group (p = .95). Overall, this study displayed no difference with regard to OS or PFS between treatment groups.
Gamboa-Vignolle et al7 performed a phase II randomized controlled trial in 2012 studying the role of chemotherapy plus WBRT (G1) versus WBRT alone (G2) in patients with brain metastases. The study enrolled 55 adult patients with KPS ≥ 50. The patients received WBRT at a total dose of 30 Gy in 10 fractions over 2 weeks. Temozolomide was the chemotherapeutic agent and was given at a dose between 200-300 mg/m 2 1 hour prior to WBRT. The study enrolled 28 patients in the G1 group and 27 patients in the G2 group. The Overall Response Rate (ORR) was 78.6% in the G1 group and 48.1% in the G2 group (p = .019). The median PFS was 11.8 months in the G1 group and 5.6 months in the G2 group (p = .014). The median OS was 8 months in the G1 group and 8.1 months in the G2 group (p = .84). Approximately 50% of the G1 group had grade 3 or 4 lymphopenia. Overall, the G2 group displayed a significantly better response rate and median PFS; however, the median OS was not significantly different between the groups.
Schild et al.17 performed a prospective cohort study in 2010 studying the role of chemotherapy plus WBRT (G1) as compared to a retrospective cohort in patients with brain metastases from melanoma. The retrospective cohort included a chemotherapy plus WBRT group (G2) and a WBRT alone group (G3). The study enrolled 7 adult patients in the G1 group and retrospectively analyzed 14 patients in the G2 group and 39 patients in the G3 group. WBRT was given for a total dose of 3750 cGy x 15 fractions. Temozolomide was given as the chemotherapeutic at a dose of 200 mg/m 2 for 5 days every 4 weeks for up to 8 cycles. The study closed the prospective cohort as rapid systemic progression occurred in 5 of 7 patients. Median survival was 3.6 months for the G1 group, 3.8 months for the G2 group and 4.3 months for the G3 group (p = 0.5). PFS was 3 months in the G2 group and 5 months in the G3 group (p = .1). Median time to systemic failure was 3 months in the G2 group and 12 months in the G3 group (p = .4). Hematologic toxicity was seen in 64% of the G2 group and 3% of the G3 group (p < .0001). Overall, the prospective arm was closed at an early stage without efficacy. The retrospective cohort displayed no overall survival benefit with a significant increase in toxicity in the patients receiving temozolomide.
Ge et al.20 performed a phase II nonrandomized prospective trial in 2013 studying the role of chemotherapy plus WBRT (G1) versus WBRT alone (G2) in patients with brain metastases from non-small cell and small-cell lung carcinoma. The study enrolled 76 adult patients with KPS > or = to 60. The patients received a total of 40 Gy in 20 fractions. Patients received a local boost increase to 56-60 Gy. Topotecan was the chemotherapeutic with a dose of 1.75 mg/m2 given 4-6 times over 4-6 weeks. The study enrolled 38 patients in each group. The median PFS and 1- and 2-year PFS rates in the G1 group and the G2 group were 6 months, 42.8%, 21.6% and 3 months, 11.6%, 8.7%, respectively (p = .014). The 1-year intracranial control rate was 75.9% in the G1 group and 65.2% in the G2 group. The 2-year intracranial control rates were 41.6% in the G1 group and 31.2% in the G2 group (p = .049). The 1-year OS was 50.8% in the G1 group and 37.9% in the G2 group. The 2-year OS was 40.4% in the G1 group and 16.5% in the G2 group (p = .178). Bone marrow suppression was seen in 68.42% in the G1 group and 50% in the G2 group. GI toxicity was seen in 63.15% in the G1 group and 44.73% in the G2 group. Overall, despite the significant increase in PFS in the topotecan group, the study displayed no significant difference in overall survival, with an increase in toxicity in the toptecan group as compared the WBRT alone group.
Risk of bias across studies
No clear bias was noted in these studies
(3) Chemotherapy first, followed by WBRT vs WBRT first, followed by chemotherapy
One study9 met the inclusion criteria this category and provided Class I evidence. Lee et al9 performed a randomized controlled trial in 2008 evaluating the role of chemotherapy before or after WBRT in patients with NSCLC. The authors evaluated 48 adult patients with clinically silent brain metastases. WBRT was provided at a total dose of 30 Gy given in 10 fractions over 12 days. The chemotherapeutic regimen included gemcitabine at a dose of 900 mg/m2 and vinorelbine at a dose of 25 mg/m2. The G1 group received up to 6 cycles of chemotherapy prior to WBRT and enrolled 25 patients. The G2 group received WBRT and 2 weeks of rest prior to chemotherapy and enrolled 23 patients. Median follow-up was 40 months across the two groups. There was no difference in ORR between treatment groups. The PFS was 3.6 months in group G1 and 4.4 months in group G2 (p= .62). The median OS was 9.1 months for group G1 and 9.9 months for group G2 (p = .61). Overall, timing of WBRT did not produce a significant difference in survival between treatment groups.
Risk of bias across studies
No clear bias was noted in this study.
(4) Sequential or concomitant chemotherapy + WBRT
One study19 met the inclusion criteria for this category and provided Class I evidence. Liu et al19 performed a randomized controlled trial in 2010 studying the role of sequential or concomitant chemotherapy in combination with WBRT in patients with SCLC. The authors evaluated 39 adult patients. The total radiation dose was 36 Gy given over 4 weeks. The chemotherapeutic regimen included teniposide (Vm26) 60 mg/m2 and cisplatin (DDP) 20 mg/m2. The concomitant group (G1) enrolled 19 patients and the sequential group (G3) enrolled 19 patients. In the G1 group, systemic chemotherapy was initiated two weeks after WBRT. The RR was 70.0% for the G1 group and 78.9% for the G2 group (p = .52). The median OS was 10 months in the G1 group and 11 months in the G2 group (p > .05). The incidence of grade III-IV leukopenia was 5% in the G1 group and 42.11% in the G2 group (p < .05). Overall, the study displayed no survival benefit between groups with a significant increase in toxicity in the group receiving chemotherapy after WBRT.
Risk of bias across studies
No clear bias was noted in this study.
(5) WBRT + 2 concurrent chemotherapeutic regimens
One study16 met the inclusion criteria for this category and provided Class I evidence. Quantin et al16 performed a randomized phase II controlled trial in 2010 studying the role of two concurrent chemotherapeutic regimens with WBRT in patients with NSCLC. The authors evaluated 70 adult patients. The patient received WBRT with a dose of 1.8 Gy per fraction in 30 fractions. Group G1 was given the regimen of vinorelbine, ifosfamide, uromitexan, cisplatin, methylprednisolone and enrolled 37 patients. Group G2 was given the regimen of ifosfamide, urometixan, methylprednisolone and enrolled 33 patients.
The ORR was seen in 17 patients (45.9%) in the G1 group and in 11 patients (33.3%) in the G2 group (p = .28). The median OS was 8.5 months in the G1 group and 5.7 months in the G2 group (p = .82). The PFS at 6 months was 58% and at 12 months was 19.3% in the G1 group. The PFS at 6 months was 30% and at 12 months 10% in the G2 group. Overall, there was no significant difference between treatment groups with regard to OR or PFS in this study.
Risk of bias across studies
No clear bias was noted in this study.
Synthesis of Results
The primary aim of this project was to address the efficacy of chemotherapy in the treatment of brain metastases in combination with WBRT, SRS, or in isolation. The authors showed that routine use of chemotherapy following WBRT for brain metastases has not been shown to increase survival and is not recommended via a Level 1 recommendation. Ten Class I studies, including two meta-analyses, examined the role of temozolomide, vinorelbine, ifosfamide, cisplatin, topotecan, and gemcitabine. Three Class II studies examined the role of temozolomide, topotecan, teniposide, and cisplatin. All studies displayed no survival benefit. The Class I studies displayed a predominance of breast and NSCLC patients, which limits the value of this recommendation that should be applicable to all patients with brain metastases. In addition, the 2 meta-analyses only provided response rates and did not evaluate overall survival or quality of life parameters, limiting the value of these studies. The authors also showed with a Level 3 recommendation that on subgroup analysis for patients with breast cancer, patients with triple negative tumors displayed increased overall survival and increased progression-free survival for those receiving WBRT plus temozolomide as compared to WBRT alone. Statistical significance was not assessed because this subgroup analysis was not powered enough to detect any difference. Patients within subgroups of breast carcinoma are encouraged to participate in future clinical trials.
Should patients with brain metastases receive chemotherapy in addition to stereotactic radiosurgery (SRS)?
(6) Chemotherapy vs chemotherapy + WBRT vs chemotherapy + SRS
One study8 met the inclusion criteria for this category and provided Class III evidence. Kim et al8 performed a retrospective cohort study in 2010 studying the role chemotherapy (G1) versus chemotherapy plus WBRT (G2) versus chemotherapy plus SRS (G3) in patients with NSCLC. The authors evaluated 129 adult patients. All patients receiving SRS received Gamma Knife radiosurgery. SRS was given at a dose of 20 Gy for lesions with a greatest diameter of 2 cm and 18 Gy for lesions with a greatest diameter between 2-3 cm. For patients receiving WBRT, 20 Gy in 5 fractions was given to 17 patients and 30 Gy in 10 fractions was given to 10 patients. The G1 group enrolled 78 patients, the G2 group enrolled 27 patients and the G3 group enrolled 24 patients. No patients received WBRT and SRS.
For patients that initially were in the G1 group, 41 (52.5%) patients developed CNS progression, of which 14 received subsequent SRS and 27 received subsequent WBRT. Median follow-up was 30 months across treatment groups. There existed a trend toward prolonged survival for the G3 group (22.4 months) versus the G1 group (13.9 months) versus the G2 group (17.7 months) (p = .86). There was no difference in PFS with the G3 group (6.3 months) versus the G1 group (5.7 months) versus the G2 group (6.9 months) (p = .68). On subgroup analysis of 110 adenocarcinoma patients, the G3 group displayed significantly favorable survival when compared with G2 group (29.3 months versus 17.7 months; p = .01) as well as when compared to the G1 group (29.3 months versus 14.6 months; p = .04). Overall, the entire group did not display a significant difference in survival between treatment groups.
Risk of bias across studies
No clear bias was noted in this study.
(7) WBRT + SRS vs chemotherapy + WBRT + SRS vs TT + WBRT + SRS
One study18 met the inclusion criteria for this sub-question and provided Class I evidence. Sperduto et al18 performed a randomized phase III controlled trial in 2013 studying the role of SRS plus WBRT (G1) versus SRS plus WBRT plus chemotherapy (G2) versus SRS plus WBRT plus targeted therapy (TT) in patients with NSCLC. The authors evaluated 125 adult patients from 28 institutions with 1-3 brain metastases < 4 cm in greatest diameter. The KPS of patients ranged between 70-100, and all patients displayed stable systemic disease. The G1 group enrolled 44 patients, the G2 group enrolled 40 patients, and the G3 group enrolled 41 patients. The chemotherapeutic was temozolomide and the TT was Erlotinib. SRS was given 14 days after the completion of WBRT. SRS was given based on the size of the lesion such that lesions < 2 cm were given 24 Gy, lesions 2.1 - 3 cm were given 18 Gy, and lesions 3.1 - 4 cm were given 15 Gy in one fraction. Temozolomide was given at a dose of 75 mg/m2 /day for 21 days with WBRT. It could then be discontinued or given at a dose of 150 mg/m2/day, 5dys/month for 6 months. Erotinib was given at a dose of 150 mg/day with WBRT or after radiation and could be continued up to 6 months.
The median follow-up was 33.6 months in this study. Median survival time for G1 was 13.4 months, for G2 was 6.3 months, and for G3 was 6.1 months. CNS progression rates were 16% for G1, 29% for G2, and 20% for G3. Median CNS PFS was 8.1 months for G1, 4.6 months for G2, and 4.8 months for G3. Deterioration rate of performance status at 6 months was 53% for G1, 86% for G2, and 86% for G3. Rate of death from neurologic cause was 17% for G1, 15% for G2, and 19% for G3. Serious grade 3-5 toxicities were 11% in G1, 41% in G2, and 49% in G3. Overall, neither the addition of temozolomide nor Erlotinib to WBRT and SRS resulted in an improvement in OS or time to CNS progression compared with WBRT and SRS alone. However, patients displayed a significant increase in toxicity with the addition of either drug.
Risk of bias across studies
No clear bias was noted in this study.
(8) Chemotherapy vs chemotherapy + SRS
One study10 met the inclusion criteria for this sub-question and provided Class I evidence. Lim et al10 performed a randomized phase III controlled trial in 2015 studying the role of SRS plus chemotherapy (G1) versus chemotherapy alone (G2) in patients with brain metastases. The authors evaluated 105 adult patients with 1-4 brain metastases < 3 cm in greatest diameter with brain edema grade 0-1. The ECOG performance status was 0-1 in all patients and all patients displayed stable systemic disease. Both treatment groups included 49 patients with > 80% of patients in each group harboring adenocarcinoma. Patients received chemotherapy within 3 weeks of SRS, and Gamma Knife radiosurgery was performed in all patients. The chemotherapeutic regimens included one of the following: (1) 60 mg/m2 cisplatin on day 1 plus 1000 mg/m 2 gemcitabine on days 1 and 8, (2) 70 mg/m2 cisplatin on day 1 plus 500 mg/m2 pemetrexed, (3) 75 mg/m2 docetaxel on day 1. (4) 60 mg/m2 cisplatin plus 175 mg/m 2 paclitaxel on day 1, (5) 60 mg/m2 cisplatin on day 1 plus 100 mg/m2 etoposide on days 1-3. In addition, cisplatin could be replaced by carboplatin.
The G1 group displayed a statistically higher number of patients with > 2 extracranial metastases (p = .026). The median follow-up was 43 months among both groups. Chemotherapy regimen 1 was the most commonly used regimen among groups. The median overall survival (OS) was 14.6 months for the G1 group and 15.3 months for the G2 group (hazard ratio 1.2). The median progression-free survival (PFS) was 9 months for the G1 group and 6.6 months for the G2 group (p = .248). The median PFS for extracranial disease was 5.4 months for both groups (p = .824). The median local PFS was not reached in the G1 group and was 10.4 months in the G2 group (p < .001). The median distal PFS was 11.9 months for the G1 group and 8.7 months for the G2 group (p = .247). The overall response rate (ORR) for cranial disease was 57% in the G1 group and 37% in the G2 group (p = .011). ORR for extracranial disease was 43% in the G1 group and 40% in the G2 group. Progressive symptomatic brain metastases 9 (18.4%) in the G1 group and 13 (26.5%) in the G2 group. Salvage SRS, chemotherapy or WBRT was higher in the G2 group but was used in both groups (p = .157). While the ORR was significantly higher in the SRS plus chemotherapy group as compared to the chemotherapy alone group, there was no statistical difference in either OS or PFS between treatment groups.
Risk of bias across studies
No clear bias was noted in this study.
Synthesis of Results
The authors showed that routine use of chemotherapy following SRS has not been shown to increase survival and is not recommended (Level 1 recommendation). Two Class I studies examined the role of cisplatin, gemcitabine, pemetrexed, docetaxel, paclitaxel, etoposide, and temodar in patients with non-small cell lung carcinoma. One Class II study examined the role of platinum-based chemotherapy in combination with either gemcitabine, docetaxel, or paclitaxel in patients with non-small cell lung carcinoma. Both the Class I and the Class II studies displayed no difference in either overall survival or progression-free survival between treatment groups as a whole. The Class II study displayed a significant difference with regard to overall and progression-free survival in lung adenocarcinoma patients receiving SRS in combination with chemotherapy as compared to other groups, from which a Level 2 recommendation based on subgroup analysis was developed. This patient population may benefit from the combination treatment, but this is to be validated in a randomized phase III trial.
Should patients with brain metastases receive chemotherapy alone?
(1) Chemotherapy vs chemotherapy + WBRT
As previously stated, four studies13-15, 21 met the inclusion criteria for this category. Three of the 4 studies provided Class I evidence (phase III randomized controlled trials). The fourth is a retrospective cohort study, providing class II evidence. Neuhaus et al. 21 performed a phase III randomized controlled trial where neither OS (p = .43) nor PFS (p = .89) differed significantly between groups. Mornex et al.13 performed a prospective randomized phase III trial and displayed no difference in brain response or local control or in overall survival between groups. Postmus et al.15 performed a phase III randomized study and displayed an improved response rate in the WBRT plus chemotherapy group with a difference in overall survival between groups. Moscetti et al.14 performed a retrospective cohort study and displayed no significant difference in progression-free or overall survival between groups. The issue of bias for each study was discussed previously for each of these studies.
(6) Chemotherapy vs chemotherapy + WBRT vs chemotherapy + SRS
Kim et al8 provided Class II evidence via a retrospective cohort study. The study displayed no difference in PFS between groups with a trend toward significance in the overall survival in the group receiving chemotherapy and SRS. The discussion of bias was performed previously.
Synthesis of Results
The authors displayed, with a Level 1 recommendation, that routine use of cytotoxic chemotherapy alone for brain metastases has not been shown to increase survival and is not recommended. Two Class I studies examined the role of fotemustine and teniposide and two Class II studies examined the role of platinum-based chemotherapy. Both of the Class I studies displayed a significantly higher median time to intracranial tumor progression in patients receiving WBRT plus chemotherapy as compared to chemotherapy alone. No difference was noted on tumor response or overall survival. Both of the Class II studies displayed no difference in overall survival in patients receiving chemotherapy alone as compared to combination treatments. This recommendation is not for emerging targeted and immune therapies addressed in the Emerging Therapy section.
CONCLUSIONS AND DISCUSSION
The use of chemotherapy in the treatment of brain metastases has been explored in a limited number of randomized controlled trials, limiting the utility of the recommendations generated by this review. Furthermore, the majority of studies included primarily patients with either breast or lung carcinoma. The studies analyzing the role of stereotactic radiosurgery included only patients with NSCLC. In addition, many of the trials do not account for prior treatment with chemotherapy. Primary endpoints also varied between trials, such that some studies looked at overall and progression-free survival while other studies looked at response rate. Statistically significant results were also not found in many of the trials, limiting the value of the acquired data. This is especially true in quantifying the value of subgroup analysis. While definitive treatment decisions are difficult to provide using the available literature, the conclusions are presented in an effort to help clinicians make informed decisions for their patients. The sub-question analysis was essentially used to answer three primary questions. These include the role of chemotherapy alone, chemotherapy plus WBRT, and chemotherapy plus SRS for the treatment of patients with brain metastases. Major conclusions from these studies include:
1. The lack of clear and robust survival benefit with cytotoxic chemotherapeutic agents alone.
2. The lack of clear and robust survival benefit with the addition of cytotoxic chemotherapy to WBRT.
3. The lack of clear and robust survival benefit with the addition of cytotoxic chemotherapy to SRS.
4. In terms of secondary endpoints, such time to neurologic progression, the data and results are mixed and do not permit robust conclusions.
5. In one trial, patients with brain metastases from lung adenocarcinoma displayed a statistically significant survival benefit with the addition of chemotherapy to SRS as compared to chemotherapy alone.
6. In one trial, patients with triple negative breast carcinoma displayed a survival benefit with the combination of chemotherapy to WBRT as compared to WBRT alone, although statistical significance was not addressed.
7. Two trials provide evidence that outcome is similar between patients receiving chemotherapy before, after, or in concomitant fashion with WBRT. However, the data remains too limited to support definitive recommendations for the delay of radiation therapy.
Potential Conflicts of Interest
The Brain Metastases Guideline Update Task Force members were required to report all possible conflicts of interest (COIs) prior to beginning work on the guideline, using the COI disclosure form of the AANS/CNS Joint Guidelines Review Committee, including potential COIs that are unrelated to the topic of the guideline. The CNS Guidelines Committee and Guideline Task Force Chair reviewed the disclosures and either approved or disapproved the nomination. The CNS Guidelines Committee and Guideline Task Force Chair are given latitude to approve nominations of task force members with possible conflicts and address this by restricting the writing and reviewing privileges of that person to topics unrelated to the possible COIs. The conflict of interest findings are provided in detail in the companion introduction and methods manuscript (here).
Disclosures
These evidence-based clinical practice guidelines were funded exclusively by the Congress of Neurological Surgeons and the Tumor Section of the Congress of Neurological Surgeons and the American Association of Neurological Surgeons, which received no funding from outside commercial sources to support the development of this document.
ACKNOWLEDGEMENTS
The authors acknowledge the CNS Guidelines Committee for its contributions throughout the development of the guideline and the AANS/CNS Joint Guidelines Review Committee for its review, comments, and suggestions throughout peer review, as well as Trish Rehring, MPH, CHES, CNS Guidelines Senior Manager, and Mary Bodach, MLIS, Senior Guidelines Specialist, for their assistance. Throughout the review process, the reviewers and authors were blinded from one another. At this time, the guidelines task force would like to acknowledge the following individual peer reviewers for their contributions: Manish Aghi, MD, PhD, Manmeet Ahuwalia, MD, Sepideh Amin-Hanjani, MD, Edward Avila, MD, Maya Babu, MD, MBA, Kimon Bekelis, MD, Priscilla Brastianos, MD, Paul Brown, MD, Andrew Carlson, MD, MS, Justin Jordan, MD, Terrence Julien, MD, Cathy Mazzola, MD, Adair Prall, MD, Shayna Rich, MD, PhD, Arjun Sahgal, MD, Erik Sulman, MD, May Tsao, MD, Michael Voglebaum, MD, Stephanie Weiss, MD, and Mateo Ziu, MD.
FIGURE 1. PRISMA diagram showing flow of study evaluation for inclusion
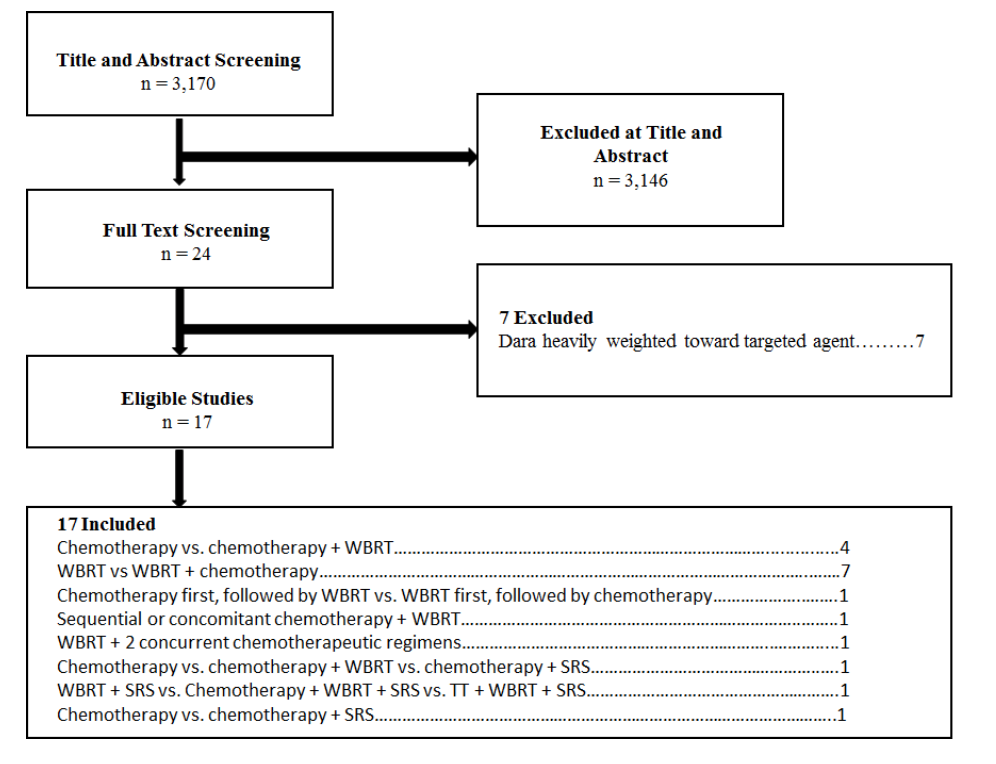
Table 1 . Chemotherapy
|
Author, Year
|
Description of Study
|
Data Class
|
Conclusions
|
|
Mornex et al,13 2003
|
Study description:
Phase III RCT comparing Chemotherapy vs chemotherapy + WBRT
Patient population:
Pts with BM from
melanoma
Treatment regimen:
G1: Fotemustine (n = 39)
G2: Fotemustine + WBRT
(n = 37)
|
I
|
Median survival:
G1: 86 days
G2: 105 days (survival
curves: log-rank; p = NS)
Tumor response:
Response rate in brain at day 50
(by ITT)
G1: OR 5.1% (CR 0/39, PR 2/39)
G2: OR 8.1% (CR 0/37, PR 3/37) (p = NS)
Median time to progression/ recurrence
Median time to progression in brain:
G1: 49 days
G2: 80 days (BM progression-free curves; Wilcoxon: p = .03; log-rank:
p = .069)
|
|
Postmus et al,15 2000
|
Study description:
Phase III RCT comparing Chemotherapy vs chemotherapy + WBRT
Patient population:
Pts with BM from
small cell lung cancer
Treatment regimen:
G1: Teniposide (n = 60)
G2: Teniposide + WBRT (n = 60)
|
I
|
Median survival:
G1: 3.2 months
G2: 3.5 months (survival
curves: log-rank; p = NS)
Tumor response:
Response rate in brain: (by ITT)
G1: OR 22% (CR 5/60, PR 8/60)
G2: OR 57% (CR 18/60, PR 16/60) (P= .001)
Response rate outside the brain:
G1: OR 20% (CR 3/60, PR 9/60)
G2: OR 33% (CR 6/60, PR 14/60) (p = NS)
Median time to progression/ recurrence
Median time to progression in brain:
NR
Significant difference in favor of G2
(BM progression-free curves: log-rank; p = .005)
|
|
Moscetti et al,14 2007
|
Study description:
Retrospective cohort study comparing Chemotherapy vs chemotherapy + WBRT
Patient population:
Pts with BM from non-small cell lung cancer
Treatment regimen:
G1: Platinum-based chemotherapy
(n = 110)
G2: WBRT+ chemotherapy (n = 46)
|
II
|
Median survival:
G1: 10 months
G2: 14 months (survival
curves: test not specified;
p = .07; NS)
Tumor response:
Response rate in brain: (OR by
ITT)
G1: OR 27.3% (CR 15/107, PR 15/107)
G2: OR 34.8% (CR 2/46, PR 14/46) (p = NS)
Extra-cranial response rate:
G1: OR 34.5% (CR 0/107, PR 38/107)
G2: OR 41.3% (CR 0/46, PR 19/46) (p = NS)
Median time to progression/ recurrence
Median progression-free survival:
G1: 6 months
G2: 6 months (Progression-free
curves: test not specified; p = NS)
|
|
Kim et al,8 2010
|
Study description:
Retrospective cohort study comparing Chemotherapy vs chemotherapy + WBRT vs chemotherapy + SRS
Patient population:
Pts with BM from non-small cell lung carcinoma
Treatment regimen:
G1: Chemotherapy
(n = 78)
G2: WBRT+ chemotherapy (n = 27)
G3: SRS + chemotherapy (n = 24)
|
II
|
Median survival:
Overall
G1: 13.9 months
G2: 17.7 months
G3: 22.4 months (p = .86)
Adenocarcinoma
G1: 14.6 months
G2: 17.7 months
G3: 29.3 months
G1 vs G3 (p = .04)
G2 vs G3 (p = .01)
Progression-free survival:
G1: 5.7 months
G2: 6.9 months
G3: 6.3 months
(p = .68)
|
BM, brain metastases; NS, not significant; Pts, patients; PFS, progression-free survival; RCT, randomized controlled trial; SRS, stereotactic radiosurgery; WBRT, whole brain radiation therapy
id="chapter5Table2"Table 2 . Whole Brain Radiotherapy
|
Author, Year
|
Description of Study
|
Data Class
|
Conclusions
|
|
Cao et al,5 2015
|
Study description:
Phase II RCT comparing chemotherapy + WBRT vs WBRT
Patient population:
Pts with BM form breast carcinoma
Treatment regimen:
G1: WBRT (n = 47)
G2: Temozolomide + WBRT (n = 37)
|
I
|
Response rate:
G1: 36%
G2: 30% (p = NS)
Median survival:
G1: 11.1 months
G2: 9.4 months (p = NS)
Median PFS:
G1: 7.4 months
G2: 6.8 months (p = NS)
Tumor subtypes:
HER2+ survival
G1: 16.1 months
G2: 20.2 months
HER2+ PFS
G1: 15 months
G2: 13.1 months
Hormone + survival
G1: 9.3 months
G2: 9.4 months
Hormone + PFS
G1: 6.7 months
G2: 5.1 months
Triple – survival
G1: 4.9 months
G2: 9.2 months
Triple - PFS
G1: 2.8 months
G2: 8.0 months
|
|
Quantin et al,16 2010
|
Study description:
Phase II RCT comparing 2 concurrent chemoradiotherapy regimens
Patient population:
Pts with BM from NSCLC
Treatment regimen:
G1:WBRT + ifosfamide, vinorelbine, and cisplatin (n = 37)
G2: WBRT + ifosfamide (n = 33)
|
I
|
Response rate:
G1: 45.9%
G2: 33.3% (p = .28)
Survival:
G1: 8.5 months
G2: 5.7 months (p = .82)
PFS:
G1: 6 months 58% 12 months 19.3%
G2: 6 months 30% 12 months 10% (p = NS)
|
|
Chua et al,6 2010
|
Study description:
Phase II RCT comparing chemotherapy + WBRT vs placebo + WBRT
Patient population:
Pts with BM from NSCLC
Treatment regimen
G1: temozolomide + WBRT (n = 47)
G2: placebo + WBRT (n = 48)
|
I
|
Number pts with BM at presentation:
G1: 30%
G2: 13% (p < .47)
Median survival:
G1: 4.4 months
G2: 5.7 months (p = .59)
Median CNS PFS:
G1: 3.1 months
G2: 3.8 months (p = .95)
|
|
Gamboa-Vignolle et al,7 2012
|
Study description:
Phase II RCT comparing chemotherapy + WBRT vs WBRT
Patient population
Pts with BM
Treatment regimen:
G1: temozolomide + WBRT (n = 28)
G2: WBRT (n = 27)
|
I
|
Breast Carcinoma:
G1: 71%
G2: 52%
Response rate:
G1: 78.6%
G2: 48.1% (p = .019)
Median PFS:
G1: 11.8 months
G2: 5.6 months (p = .014)
Median survival:
G1: 8 months
G2: 8.1 months (p = .84)
Approximately 50% of G1 had grade 3 or 4 lymphopenia
|
|
Ge et al,20 2013
|
Study description:
Prospective phase II nonrandomized trial comparing chemotherapy + WBRT vs WBRT
Patient population:
Pts with BM from lung carcinoma
Treatment regimen:
G1: topotecan + WBRT (n = 38)
G2: WBRT (n = 38)
|
II
|
PFS:
G1: 6 months
G2: 3 months
1-year PFS:
G1: 42.8%
G2: 11.6%
2-year PFS:
G1: 21.6%
G2: 8.7% (p = .014)
1-year intracranial control rate:
G1: 75.9%
G2: 65.2%
2-year intracranial control rate:
G1: 41.6%
G2: 31.2% (p = .049)
1-year survival:
G1: 50.8%
G2: 37.9%
2-year survival:
G1: 40.4%
G2: 16.5% (p = .178)
Bone marrow suppression:
G1: 68.42%
G2: 50%
Gastrointestinal toxicity:
G1: 63.15%
G2: 44.73%
|
|
Lee et al,9 2008
|
Study description:
RCT comparing WBRT before or after chemotherapy
Patient population:
Pts with BM from NSCLC
Treatment regimen:
G1: Chemotherapy (up to 6 cycles prior) + WBRT (n = 25)
G2: WBRT (2 weeks of rest prior) + chemotherapy (n = 23)
|
I
|
Response rate:
G1 = G2
PFS:
G1: 3.6 months
G2: 4.4 months (p = .62)
Median survival:
G1: 19.1 months
G2: 9.9 months (p = .61)
|
|
Liu et al,19 2010
|
Study description:
RCT comparing sequential or concomitant chemotherapy + WBRT
Patient population:
Pts with BM from SCLC
Treatment regimen:
G1: Chemotherapy at same time as WBRT (n = 19)
G2: Chemotherapy 2 weeks after WBRT (n = 20)
|
I
|
Response rate:
G1: 70.0%
G2: 78.9% (p = .52)
Median survival:
G1: 10 months
G2: 11 months (p > .05)
Grade III-IV leukopenia
G1: 5%
G2: 42.11% (p < .05)
|
|
Neuhaus et al,21 2009
|
Study population:
Phase III RCT comparing chemotherapy + WBRT vs chemotherapy
Patient population:
Pts with BM from lung carcinoma
Treatment regimen:
G1: Topotecan + WBRT (n = 47)
G2: WBRT (n = 49)
|
I
|
Neither overall survival (p = .43) or PFS (p = .89) differed significantly between groups
True for both NSCLC and SCLC
Study stopped at interim analysis
|
|
Schild et al,17 2010
|
Study population:
Prospective cohort study comparing chemotherapy + WBRT vs WBRT
Patient population:
Pts with BM from melanoma
Treatment regimen:
G1: Prospective group temozolomide + WBRT (n = 7)
G2: Retrospective group temozolomide + WBRT (n = 14)
G3: Retrospective group WBRT (n = 39)
|
II
|
Median survival:
G1: 3.6 months
G2: 4.3 months
G3: 3.8 months (p = NS)
Study closed for G1 as rapid systemic progression in 5/7 pts
PFS:
G2: 3 months
G3: 5 months (p = .1)
Median systemic failure G2: 3 months
G3: 12 months (p = .4)
Toxicity:
G2: 64%
G3: 3% (p < .0001)
|
|
Sperduto et al,18 2013
|
Study description:
Phase III RCT comparing chemotherapy + WBRT vs chemotherapy + WBRT + SRS
Patient population:
Pts with BM from NSCLC
Treatment regimen:
G1: WBRT + SRS
(n = 44)
G2: WBRT+ SRS + temozolomide (n = 40)
G3: WBRT + SRS + erlotinib (n = 41)
|
I
|
Median survival:
G1: 13.4 months
G2: 6.3 months
G3: 6.1 months (p = NS)
Median progression-free survival:
G1: 8.1 months
G2: 4.6 months
G3: 4.8 months
Deterioration rate of performance status at 6 months:
G1: 53%
G2: 86%
G3: 86%
G1 vs G2 (p = .002)
G1 vs G3 (p < .001)
Rate of death of neurologic cause:
G1: 17%
G2: 15%
G3: 19% (p = NS)
Serious grade 3-5 toxicities:
G1: 11%
G2: 41%
G3: 49% (p < .001)
|
|
Kim et al,8 2010
|
Study description:
Retrospective cohort study comparing chemotherapy vs chemotherapy + WBRT vs chemotherapy + SRS
Patient population:
Pts with BM from NSCLC
Treatment regimen:
G1: Chemotherapy (n = 78)
G2: WBRT + chemotherapy (n = 27)
G3: SRS + chemotherapy (n = 24)
|
II
|
Median survival:
Overall
G1: 13.9 months
G2: 17.7 months
G3: 22.4 months (p = .86)
Adenocarcinoma
G1: 14.6 months
G2: 17.7 months
G3: 29.3 months
G1 vs G3 (p = .04)
G2 vs G3 (p = .01)
ORR
G1: 53.7%
G2: 58.6%
G3:68.8% (p = .05)
|
BM, brain metastases; DDP, cisplatin; NSCLC, non-small cell lung carcinoma; NS, not significant; ORR, objective response rate; Pts, patients; PFS, progression-free survival; RCT, randomized controlled trial; SCLC, small cell lung carcinoma; SRS, stereotactic radiosurgery; Vm26, teniposide; WBRT, whole brain radiation therapy
id="chapter5Table3"Table 3 . Stereotactic Radiosurgery
|
Author, Year
|
Description of Study
|
Data Class
|
Conclusions
|
|
Lim et al,10 2015
|
Study description:
Phase III RCT comparing Chemotherapy vs chemotherapy + SRS
Patient population:
105 adult patients with BM from NSCLC
Treatment regimen:
G1: Chemotherapy + SRS (n = 49)
G2: Chemotherapy (N=49)
Chemotherapy
Cisplatin + Gemcitabine
Cisplatin + Pemetrexed
Docetaxel
Cisplatin + Paclitaxel
Cisplatin + Etoposide
|
I
|
G1: Greater patients with > 2 metastases (p = .026)
Median survival:
G1: 14.6 months
G2: 15.4 months (p = NS)
Median PFS:
G1: 9.0 months
G2: 6.6 months (p = .248)
Median local PFS:
G1: Not reached
G2: 10.5 months (p < .001)
Median distal PFS:
G1: 11.9 months
G2: 8.7 months (p = .247)
ORR cranial disease:
G1: 57%
G2: 37% (p = .011)
ORR extracranial disease:
G1: 43%
G2: 40% (p = NS)
|
|
Sperduto et al,18 2013
|
Study description:
Phase III RCT comparing Chemotherapy + WBRT vs chemotherapy + WBRT + SRS
Patient population:
Pts with BM from NSCLC
Treatment regimen:
G1: WBRT + SRS
(n = 44)
G2: WBRT+ SRS + temozolomide (n = 40)
G3: WBRT + SRS + erlotinib (n = 41)
|
I
|
Median survival:
G1: 13.4 months
G2: 6.3 months
G3: 6.1 months (p = NS)
Median progression-free survival:
G1: 8.1 months
G2: 4.6 months
G3: 4.8 months
Deterioration rate of performance status at 6 months:
G1: 53%
G2: 86%
G3: 86%
G1 vs G2 (p = .002)
G1 vs G3 (p < .001)
Rate of death of neurologic cause:
G1: 17%
G2: 15%
G3: 19% (p = NS)
Serious grade 3-5 toxicities:
G1: 11%
G2: 41%
G3: 49% (p < .001)
|
|
Kim et al,8 2010
|
Study description:
Retrospective cohort study comparing Chemotherapy vs chemotherapy + WBRT vs chemotherapy + SRS
Patient population:
Pts with BM from NSCLC
Treatment regimen:
G1: Chemotherapy (n = 78)
G2: WBRT+ chemotherapy (n = 27)
G3: SRS + chemotherapy (n = 24)
|
III
|
Median survival:
Overall
G1: 13.9 months
G2: 17.7 months
G3: 22.4 months (p = .86)
Adenocarcinoma
G1: 14.6 months
G2: 17.7 months
G3: 29.3 months
G1 vs G3 (p = .04)
G2 vs G3 (p = .01)
ORR
G1: 53.7%
G2: 58.6%
G3:68.8% (p = .05)
|
BM, brain metastases; NSCLC, non-small cell lung carcinoma; NS, not significant; ORR, objective response rate; RCT, randomized controlled trial; SRS, stereotactic radiosurgery; WBRT, whole brain radiation therapy
REFERENCES
1. Gavrilovic IT, Posner JB. Brain metastases: epidemiology and pathophysiology. J Neurooncol. Oct 2005;75(1):5-14.
2. Mehta MP, Paleologos NA, Mikkelsen T, et al. The role of chemotherapy in the management of newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol. Jan 2010;96(1):71-83.
3. Gerstner ER, Fine RL. Increased permeability of the blood-brain barrier to chemotherapy in metastatic brain tumors: establishing a treatment paradigm. J Clin Oncol. Jun 1 2007;25(16):2306-2312.
4. Halasz LM, Uno H, Hughes M, et al. Comparative effectiveness of stereotactic radiosurgery versus whole-brain radiation therapy for patients with brain metastases from breast or non-small cell lung cancer. Cancer. Jul 01 2016;122(13):2091-2100.
5. Cao KI, Lebas N, Gerber S, et al. Phase II randomized study of whole-brain radiation therapy with or without concurrent temozolomide for brain metastases from breast cancer. Ann Oncol. Jan 2015;26(1):89-94.
6. Chua D, Krzakowski M, Chouaid C, et al. Whole-brain radiation therapy plus concomitant temozolomide for the treatment of brain metastases from non-small-cell lung cancer: a randomized, open-label phase II study. Clin Lung Cancer. May 2010;11(3):176-181.
7. Gamboa-Vignolle C, Ferrari-Carballo T, Arrieta O, Mohar A. Whole-brain irradiation with concomitant daily fixed-dose temozolomide for brain metastases treatment: a randomised phase II trial. Radiother Oncol. Feb 2012;102(2):187-191.
8. Kim KH, Lee J, Lee JI, et al. Can upfront systemic chemotherapy replace stereotactic radiosurgery or whole brain radiotherapy in the treatment of non-small cell lung cancer patients with asymptomatic brain metastases? Lung Cancer. May 2010;68(2):258-263.
9. Lee DH, Han JY, Kim HT, et al. Primary chemotherapy for newly diagnosed nonsmall cell lung cancer patients with synchronous brain metastases compared with whole-brain radiotherapy administered first : result of a randomized pilot study. Cancer. Jul 1 2008;113(1):143-149.
10. Lim SH, Lee JY, Lee MY, et al. A randomized phase III trial of stereotactic radiosurgery (SRS) versus observation for patients with asymptomatic cerebral oligo-metastases in non-small-cell lung cancer. Ann Oncol. Apr 2015;26(4):762-768.
11. Liu R, Wang X, Ma B, Yang K, Zhang Q, Tian J. Concomitant or adjuvant temozolomide with whole-brain irradiation for brain metastases: a meta-analysis. Anticancer Drugs. Jan 2010;21(1):120-128.
12. Liu WJ, Zeng XT, Qin HF, Gao HJ, Bi WJ, Liu XQ. Whole brain radiotherapy plus chemotherapy in the treatment of brain metastases from lung cancer: a meta-analysis of 19 randomized controlled trails. Asian Pac J Cancer Prev. 2012;13(7):3253-3258.
13. Mornex F, Thomas L, Mohr P, et al. A prospective randomized multicentre phase III trial of fotemustine plus whole brain irradiation versus fotemustine alone in cerebral metastases of malignant melanoma. Melanoma Res. Feb 2003;13(1):97-103.
14. Moscetti L, Nelli F, Felici A, et al. Up-front chemotherapy and radiation treatment in newly diagnosed nonsmall cell lung cancer with brain metastases: survey by Outcome Research Network for Evaluation of Treatment Results in Oncology. Cancer. Jan 15 2007;109(2):274-281.
15. Postmus PE, Haaxma-Reiche H, Smit EF, et al. Treatment of brain metastases of small-cell lung cancer: comparing teniposide and teniposide with whole-brain radiotherapy--a phase III study of the European Organization for the Research and Treatment of Cancer Lung Cancer Cooperative Group. J Clin Oncol. Oct 1 2000;18(19):3400-3408.
16. Quantin X, Bozonnat MC, Pujol JL. Recursive Partitioning Analysis Groups II-III brain metastases of non-small cell lung cancer: a phase II randomized study comparing two concurrent chemoradiotherapy regimens. J Thorac Oncol. Jun 2010;5(6):846-851.
17. Schild SE, Behl D, Markovic SN, et al. Brain metastases from melanoma: is there a role for concurrent temozolomide in addition to whole brain radiation therapy? Am J Clin Oncol. Dec 2010;33(6):633-636.
18. Sperduto PW, Wang M, Robins HI, et al. A phase 3 trial of whole brain radiation therapy and stereotactic radiosurgery alone versus WBRT and SRS with temozolomide or erlotinib for non-small cell lung cancer and 1 to 3 brain metastases: Radiation Therapy Oncology Group 0320. Int J Radiat Oncol Biol Phys. Apr 1 2013;85(5):1312-1318.
19. Liu M ZY, Han Q, Gao T, Luo Z, Wang W. Whole brain radiotherapy concomitant or sequential Vm26/DDP in treating small cell lung cancer patients with brain metastases. Chinese-German Journal of Clinical Oncology. 2010;9(1):17-21.
20. Ge XH, Lin Q, Ren XC, et al. Phase II clinical trial of whole-brain irradiation plus three-dimensional conformal boost with concurrent topotecan for brain metastases from lung cancer. Radiat Oncol. 2013;8:238.
21. Neuhaus T, Ko Y, Muller RP, et al. A phase III trial of topotecan and whole brain radiation therapy for patients with CNS-metastases due to lung cancer. Br J Cancer. Jan 27 2009;100(2):291-297.
APPENDIX A
Search 1: BNC_SRS
The Cochrane Databases of Systematic Reviews
- MeSH descriptor [Brain Neoplasms] explode all trees
- ((brain or brainstem or intracranial or posterior fossa) and (cancer* or carcinoma* or tumor* or tumour* or neoplasm*))
- MeSH descriptor [Neoplasm Metastasis] explode all trees
- metastas*
- (1 or 2)
- (3 or 4)
- (5 and 6)
- MeSH descriptor [Drug Therapy] explode all trees
- drug therap*
- chemotherap*
- antineoplastic
- anticancer drug*
- (8 or 9 or 10 or 11 or 12)
- MeSH descriptor [Radiosurgery] explode all trees
- radiosurg*
- stereotactic radiotherap*
- stereotactic surger*
- stereotaxic technique*
- SRS
- (14 or 15 or 16 or 17 or 18 or 19)
- (7 and 13 and 20)
Publication Year from 2008 to 2015, in Cochrane Reviews (Reviews and Protocols), Other Reviews, Trials, Methods Studies, Technology Assessments, Economic Evaluations and Cochrane Groups
Results: 43
PubMed (MEDLINE)
- exp Brain Neoplasms/
- ((brain or brainstem or intracranial or posterior fossa) and (cancer* or carcinoma* or tumor* or tumour* or neoplasm*)).mp.
- exp Neoplasm Metastasis/
- metastas*.mp.
- (1 or 2)
- (3 or 4)
- (5 and 6)
- exp Drug Therapy/
- drug therap*.mp.
- Chemotherap*.mp.
- antineoplastic.mp.
- anticancer drug*.mp.
- (8 or 9 or 10 or 11 or 12)
- exp Radiosurgery/
- Radiosurg*.mp.
- Stereotactic radiotherap*.mp.
- stereotactic surger*.mp.
- stereotaxic technique*.mp.
- SRS.mp.
- (14 or 15 or 16 or 17 or 18 or 19)
- (7 and 13 and 20)
- limit 21 to (english language and humans and yr=”1990-2015”)
- limit 22 to (case reports or letter or “review”)
- (22 not 23)
Results: 192
Search 2: BNC_WBRT
The Cochrane Databases of Systematic Reviews
- MeSH descriptor [Brain Neoplasms] explode all trees
- ((brain or brainstem or intracranial or posterior fossa) and (cancer* or carcinoma* or tumor* or tumour* or neoplasm*))
- MeSH descriptor [Neoplasm Metastasis] explode all trees
- metastas*
- (1 or 2)
- (3 or 4)
- (5 and 6)
- MeSH descriptor [Drug Therapy] explode all trees
- drug therap*
- chemotherap*
- antineoplastic
- anticancer drug*
- (8 or 9 or 10 or 11 or 12)
- MeSH descriptor [Radiotherapy] explode all trees
- MeSH descriptor [Radiotherapy, Adjuvant] explode all trees
- radiotherap*
- radiat*
- stereotactic radiotherap*
- whole brain irradiation
- whole brain radiotherap*
- WBI
- WBRT
- whole brain radiation therap*
- (14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23)
- (7 and 13 and 24)
Publication Year from 2008 to 2015, in Cochrane Reviews (Reviews and Protocols), Other Reviews, Trials, Methods Studies, Technology Assessments, Economic Evaluations and Cochrane Groups
Results: 203
PubMed (MEDLINE)
- exp Brain Neoplasms/
- ((brain or brainstem or intracranial or posterior fossa) and (cancer* or carcinoma* or tumor* or tumour* or neoplasm*)).mp.
- exp Neoplasm Metastasis/
- metastas*.mp.
- (1 or 2)
- (3 or 4)
- (5 and 6)
- exp Drug Therapy/
- drug therap*.mp.
- Chemotherap*.mp.
- antineoplastic.mp.
- anticancer drug*.mp.
- (8 or 9 or 10 or 11 or 12)
- exp Radiotherapy/
- exp Radiotherapy, Adjuvant/
- radiotherap*.mp.
- radiat*.mp.
- Stereotactic radiotherap*.mp.
- Whole brain irradiation.mp.
- Whole brain radiotherap*.mp.
- WBI.mp.
- WBRT.mp.
- Whole brain radiation therap*.mp.
- (14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23)
- (7 and 13 and 24)
- limit 25 to (english language and humans and yr=”2008-2015”)
- limit 26 to (case reports or letter or “review”)
- (26 not 27)
Results: 483
Search 3: BNC
The Cochrane Databases of Systematic Reviews
- MeSH descriptor [Brain Neoplasms] explode all trees
- ((brain or brainstem or intracranial or posterior fossa) and (cancer* or carcinoma* or tumor* or tumour* or neoplasm*))
- MeSH descriptor [Neoplasm Metastasis] explode all trees
- metastas*
- (1 or 2)
- (3 or 4)
- (5 and 6)
- MeSH descriptor [Drug Therapy] explode all trees
- drug therap*
- chemotherap*
- antineoplastic
- anticancer drug*
- (8 or 9 or 10 or 11 or 12)
- (7 and 13)
Publication Year from 1990 to 2015, in Cochrane Reviews (Reviews and Protocols), Other Reviews, Trials, Methods Studies, Technology Assessments, Economic Evaluations and Cochrane Groups
Results: 572
PubMed (MEDLINE)
- exp Brain Neoplasms/
- ((brain or brainstem or intracranial or posterior fossa) and (cancer* or carcinoma* or tumor* or tumour* or neoplasm*)).mp.
- exp Neoplasm Metastasis/
- metastas*.mp.
- (1 or 2)
- (3 or 4)
- (5 and 6)
- exp Drug Therapy/
- drug therap*.mp.
- Chemotherap*.mp.
- antineoplastic.mp.
- anticancer drug*.mp.
- (8 or 9 or 10 or 11 or 12)
- (7 and 13)
- limit 14 to (english language and humans and yr=”1990-2015”)
- limit 15 to (case reports or letter or “review”)
- (15 not 16)
Results: 1959
Source: Neurosurgery