Reposted with permission from ©AANS, 2014
J Neurosurg Pediatrics (Suppl) 14:24–29, 2014
AANS, 2014
(Original text of the guideline was edited to reflect the update. Please click here for the original publication.)
Pediatric hydrocephalus: systematic literature review and evidence-based guidelines
Part 3: Endoscopic computer-assisted electromagnetic navigation and ultrasonography as technical adjuvants for shunt placement
UPDATE
Ann Marie Flannery, MD,1 Ann-Christine Duhaime, MD,2 Mandeep S. Tamber, MD, PhD,3 Joanna Kemp, MD1
1Department of Neurological Surgery, Saint Louis University, St. Louis, Missouri; 2Department of Pediatric Neurosurgery, Massachusetts General Hospital, Boston, Massachusetts; and 3Department of Pediatric Neurological Surgery, Children’s Hospital of Pittsburgh, University of Pittsburgh, Pittsburgh, Pennsylvania
Object. This systematic review was undertaken to answer the following question: Do technical adjuvants such as ventricular endoscopic placement, computer-assisted electromagnetic guidance, or ultrasound guidance improve ventricular shunt function and survival?
Methods. The US National Library of Medicine PubMed/MEDLINE database and the Cochrane Database of Systematic Reviews were queried using MeSH headings and key words specifically chosen to identify published articles detailing the use of cerebrospinal fluid shunts for the treatment of pediatric hydrocephalus. Articles meeting specific criteria that had been delineated a priori were then examined, and data were abstracted and compiled in evidentiary tables. These data were then analyzed by the Pediatric Hydrocephalus Systematic Review and EvidenceBased Guidelines Task Force to consider evidence-based treatment recommendations.
Results. The search yielded 163 abstracts, which were screened for potential relevance to the application of technical adjuvants in shunt placement. Fourteen articles were selected for full-text review. One additional article was selected during a review of literature citations. Eight of these articles were included in the final recommendations concerning the use of endoscopy, ultrasonography, and electromagnetic image guidance during shunt placement, whereas the remaining articles were excluded due to poor evidence or lack of relevance.
The evidence included 1 Class I, 1 Class II, and 6 Class III papers. An evidentiary table of relevant articles was created.
Conclusions. Recommendation: There is insufficient evidence to recommend the use of endoscopic guidance for routine ventricular catheter placement. Strength of Recommendation: Level I, high degree of clinical certainty.
Recommendation: The routine use of ultrasound-assisted catheter placement is an option. Strength of Recommendation: Level III, unclear clinical certainty.
Recommendation: The routine use of computer-assisted electromagnetic (EM) navigation is an option. Strength of Recommendation: Level III, unclear clinical certainty.
(http://thejns.org/doi/abs/10.3171/2014.7.PEDS14323)
Key Words: cerebrospinal fluid shunt, hydrocephalus, ultrasonography, ventricular catheter, ventricular shunt, computer-assisted navigation, image-guided navigation, electromagnetic guidance, endoscopy, practice guidelines
Abbreviations used in this paper: AANS = American Association of Neurological Surgeons; CNS = Congress of Neurological Surgeons; EM = electromagnetic ; ETV = endoscopic third ventriculostomy.
As navigation, imaging, and endoscopy have increasingly been used in the field of neurosurgery, they have been applied to the placement of CSF shunts. Surgeons have used these technical adjuvants in attempts to accomplish good catheter placement with the hopes of improving the longevity of the shunt as well as reducing potential complications. This specific systematic review was undertaken to answer the following question: Do technical adjuvants such as ventricular endoscopic placement, computer-assisted elect romagnetic (EM) guidance, or ultrasound guidance improve ventricular shunt function and survival? As seen in the following Methods section, we conducted a search for articles on the use of CSF shunts in pediatric patients with hydrocephalus. The original search yielded 163 abstracts, which were screened for their potential relevance to the application of technical adjuvants in shunt placement. Fifteen articles were deemed relevant. Eight of these articles were included in the final recommendations for the use of endoscopy, ultrasonography, or EM image guidance in the placement of shunts, with the remainder excluded due to poor evidence or lack of relevance.
Authors performed an update of the original search yielding 118 citations, of which 8 were selected for full text review. Four studies were included, confirming the original recommendations. The remainder were excluded.
Methods
The US National Library of Medicine PubMed/ MED LINE database and the Cochrane Database of Systematic Reviews were queried for the period January 1966 through March 2012 using MeSH headings and key words specifically chosen to identify published articles detailing the use of CSF shunts for the treatment of pediatric hydrocephalus. Please see below for the specific search terms and strategies used (Fig. 1).
Authors performed an updated literature search (in PubMed and Cochrane Central) for this guideline chapter through a medical librarian at the Congress of Neurological Surgeons Guidelines office using the below-mentioned existing search terms to update the original search through November 30, 2019 (Figure 2).
Search Terms
PubMed/MEDLINE
- (“Cerebrospinal Fluid Shunts”[MeSH]) AND “Hydrocephalus”[MeSH:noexp]
- Limit 1 to Child (0–18 years)
- 2 and ((ventricular AND (catheter OR shunt)) AND (“computer assisted” OR “image guided” OR electromagnetic OR ultrasound OR Endoscopy[MeSH] OR endoscop*))
- Limit to English and Humans
Cochrane Database
- MeSH descriptor Child
- MeSH descriptor Infant
- 1 or 2 and (MeSH descriptor Cerebrospinal Fluid
Shunts)
- 3 and (MeSH descriptor Hydrocephalus)
- 4 and (ventricular NEAR/2 (catheter OR shunt))
- (computer OR ultrasound OR endoscop*)
- 5 and 6
Search Strategies
Articles meeting specific criteria that had been delineated a priori were then examined, and the data yielded were abstracted and compiled in evidentiary tables (Tables 1–4). These data were then analyzed by the Pediatric Hydrocephalus Systematic Review and Evidence-Based Guidelines Task Force to consider evidence-based treatment recommendations.
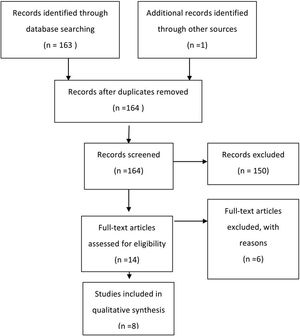
Fig. 1. Flowchart showing the process involved in identifying relevant literature.
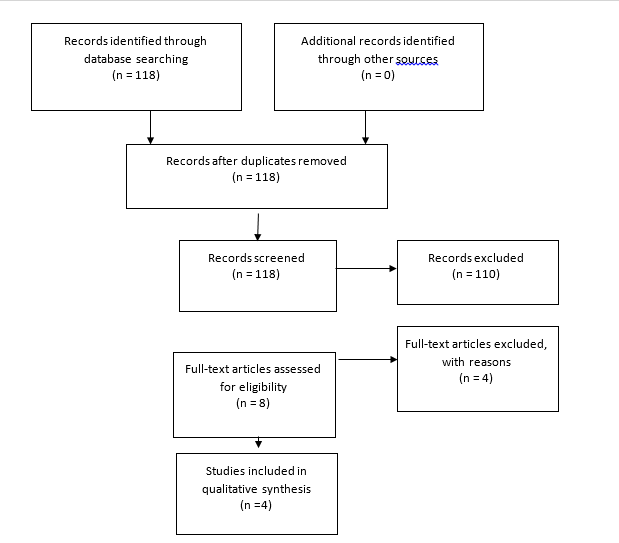
Fig. 2. Flowchart showing the process involved in identifying relevant literature for the 2020 Update. The criteria for “records excluded” and “full text articles excluded with reasons” are detailed in Part 1 of the Guidelines.
Results
Endoscopy
Recommendation: There is insufficient evidence to recommend using endoscopic guidance for routine ventricular catheter placement. Strength of Recommendation: Level I, high degree of clinical certainty.
Four studies were identified to assess the use of endoscopy in the placement of ventricular catheters (Table 1). Two of the earlier reports in the literature described a case series by Vries1 and another by Kellnar et al.2 Vries1 described the technique for insertion of endoscopically placed catheters and reported that 79% of patients for whom endoscopy was used did not require further shunt revision. However, the author did not report the follow-up period, and without a control arm there is no clear demonstration of an advantage of using the endoscope over the standard technique, which relies on anatomical landmarks. Kellnar et al.2 described a case series in which neuroendoscopy was used for placement of ventricular catheters in 14 patients. These authors demonstrated the feasibility of their technique and stated that there were no revisions due to catheter malposition during an 18-month followup period.2 Again, without a control group, no conclusions can be drawn regarding an advantage of endoscopic shunt insertion over standard techniques.
A later study by Villavicencio et al3 retrospectively compared the survival of shunts placed with neuroendoscopic guidance to that of shunts placed without guidance. The authors found no advantage to overall shunt survival between the two study groups (hazard ratio 1.08, 95% CI 0.84–1.41). They did, however, note that the risk of proximal failure was lower in the endoscopy group (odds ratio 0.56, 95% CI 0.32–0.93) and observed an increased rate of distal malfunction when compared with shunts placed without endoscopic assistance.
The strongest evidence that the routine use of endoscopic placement did not improve outcome was reported by Kestle and colleagues4 in a randomized controlled trial in which 393 patients requiring a shunt were randomized into either an endoscopy group or a standard group. There were no significant differences in the overall shunt survival rate between the groups (p = 0.09) or in the postoperative assessment of optimal catheter placement (away from the choroid plexus). The most common cause of shunt failure was proximal obstruction in both groups.
TABLE 1: Use of endoscopy in the placement of ventricular catheters: summary of evidence*
| First Author & Year |
Study Description |
Data Class, Quality and Reasons |
Results and Conclusions |
|
Kestle et al., 2003
|
Endoscopic placement of new shunts at 16 centers, randomized to endoscope directed vs non–endoscope directed. 393 pts in study, ventricular catheter scope.
|
Class I
Randomized, blinded, multicenter.
|
Incidence of shunt failure at 1 yr: Endoscope Insertion Group: 42%; Non–Endoscopic Insertion Group: 34%.
Time to 1st shunt failure did not differ between groups (log-rank = 2.92, p = 0.09). |
|
Villavicencio et al., 2003
|
447 children underwent total of 965 shunt placements or revisions.
605 catheters (63%) placed w/ aid of endoscope; 360 catheters (37.3%) placed w/o endoscope. |
Class III
Retrospective review, historical cohort.
|
Neuroendoscopy did not independently affect risk of subsequent shunt failure (HR 1.08, 95% CI 0.84–1.41).
Endoscopic placement:
- Independently decreased odds of proximal obstruction (OR 0.56, 95% CI 0.32–0.93);
- Increased odds of distal malfunction (OR 1.52, 95% CI 1.02–2.72);
- Was not associated w/ infection (OR 1.42, 95% CI0.78–2.61).
Authors state, “Endoscope assisted ventricular catheter placement decreased the odds of proximal obstruction but failed to improve overall shunt survival in this 6-year experience.” |
|
|
Vries, 1980
|
2.7-mm 0° scope used to place ventricular catheter.
102 shunts in 85 pts, 67 were new shunts.
|
Class III
Case series, retrospective, chart review.
No statistical analysis.
|
Max follow-up 18 mos.
24 shunt malfunctions in 18 pts: 9 were ventricular catheter malfunctions. 6 infections.
Author reported that 79% of the shunts were “troublefree.” |
|
TABLE 2: Use of ultrasound guidance in the placement of ventricular catheters: summary of evidence
| First Author & Year |
Study Description |
Data Class, Quality and Reasons |
Results and Conclusions |
|
Whitehead et al., 2007
|
Authors used transcranial sonography via a 2-cm bur hole for CSF ventricular catheter insertion.
10 pts w/o open fontanelles & normal-size to slitlike ventricles, July–December 2006.
|
Class III
Case series & technical note.
|
10 of 10 catheters in ventricles.
No follow-up.
No data on shunt survival.
|
|
|
TABLE 3: Use of electromagnetic image guidance in the placement of ventricular catheters: summary of evidence
| First Author & Year |
Study Description |
Data Class, Quality and Reasons |
Results and Conclusions |
|
2010 |
|
3 centers, new shunts, adult & pediatric pts followed up for 1 yr or to shunt failure.
Graded by observer blinded to placement method.
|
Pediatric pts: 20 w/o navigation, 15 w/ EM image navigation.
|
|
Class II
Cohort, good-quality prospective study.
Follow-up for EM image navigation group was shorter (6 mos) than for no navigation group.
|
Small study, <50% pediatric pts.
|
|
Pediatric standard group (no navigation): 20 pts < 18 yrs of age. 6 shunts failed (30%); in 4 cases early failures due to proximal obstruction.
EM image navigation group: 15 children, 3 shunts failed (20%). Failures due to infection in 1 pt & valve blockage in 2 pts.
|
No significant difference in overall shunt failure in the pediatric group when EM image guidance was used for shunt placement (p = 0.39, Fisher exact test).
|
|
Levitt et al., 2012
|
|
89 pts, 102 shunt surgeries: 58 initial &
|
44 revisions. Image guidance used in 56 surgeries; standard technique used in 46 surgeries.
|
Retrospective review.
|
|
22% shunt failure rate w/ standard technique; 25% shunt failure rate w/ EM image guidance (not significant, p = 0.21, log-rank test).
Ventricle size significantly smaller in pts in EM image guidance group (p < 0.02) & in the surgery revision group (p < 0.01), Student t-test. Small ventricle size did not affect shunt failure rate, even when authors controlled for technique of insertion.
|
Image guidance significantly improved accuracy of catheter placement (p < 0.01). Shunt placement accuracy had no significant effect on shunt failure. Significant improvement in catheter position, even though pts in EM image guidance group had smaller ventricles.
|
Ultrasound Guidance
Recommendation: The routine use of ultrasound-assisted catheter placement is an option. Strength of Recommendation: Level III, unclear clinical certainty.
The supporting evidence consisted of 1 Class III study with limited follow-up and no control or comparison (Table 2).
Few studies have sought to evaluate the utility of ultrasound in the placement of ventricular catheters. One Class III cohort study with a limited follow-up and no control or comparison met the inclusion criteria and was included as evidence to support this topic. Whitehead et al5 described the technique of placing the ventricular catheter with ultrasound guidance in pediatric patients with closed fontanelles. The authors described the creation of a 2-cm bur hole, followed by catheter placement and ultrasonography to confirm catheter location. There was no analysis of outcomes related to shunt longevity, but immediate postoperative imaging did confirm the expected placement of the catheter away from the choroid plexus.5 Ultrasound-assisted catheter placement may be used to confirm placement of the proximal catheter within the cerebral ventricle.
Electromagnetic Image Guidance
Recommendation: The routine use of computer assisted electromagnetic (EM) navigation is an option. Strength of Recommendation: Level III, unclear clinical certainty.
One Class II study, which did not reach significance in the pediatric subset, and 1 Class III study, which reported a decrease in proximal failure compared with historical reports, were included as evidence to support this topic.
Electromagnetic image guidance has been used (and studied in the pediatric hydrocephalus literature) as a technical adjuvant for assisting placement of ventricular catheters. In a case series by Clark et al6 published in 2008, prospectively collected data confirmed the feasibility of using EM image guidance, specifically in 23 patients with anatomy that was difficult to navigate, including those with small and slit ventricles or complex loculated hydrocephalus. These authors demonstrated a 9% proximal revision rate in the 7-month follow-up period, which they compared with a historical control group in which there was a 35% failure rate. The authors proposed a randomized controlled trial to strengthen this evidence, as their study did not have its own control, had a short follow-up period, and included a small number of patients.
An article by Hayhurst and coauthors7 described a nonrandomized prospective cohort study in which standard shunt placement was compared with EM image– guided shunt placement in both adult and pediatric patients. The end points of the study were failure rates as well as grading of the catheter position as follows: Grade 1, catheter tip floating in CSF equidistant from the ventricle walls, away from the choroid plexus, and in a straight trajectory from the bur hole; Grade 2, catheter tip touching the ventricle wall or the choroid plexus; and Grade 3, part of the catheter tip within the parenchyma or failure to cannulate the ventricle completely. The pediatric cases were analyzed separately with regard to shunt failure, and the data showed a 30% failure rate in the standard cohort and a 20% failure rate in the EM image guidance cohort. This difference was statistically insignificant. In the entire cohort, which included both adult and pediatric patients, “the rate of proximal obstruction falls ... from 17 to 6% [when] using EM-navigated placement (p = 0.129, Fisher exact test).”7 Despite that, the overall failure rate was still equivalent, as other components of the system failed, even when the proximal catheter performance improved. There were no Grade 3 catheter positions in the EM image guidance group; this did have a significant impact on shunt survival compared with Grades 1 and 2. These data were not analyzed independently for the pediatric patients included in the study.7
A recent paper by Levitt et al8 also looked at the use of EM navigation versus standard shunt placement. The authors retrospectively analyzed 102 surgeries with frontal catheter placement in pediatric patients to identify the rates of subsequent shunt failure and catheter positioning with the same grading as previously described. The authors found no significant difference in the incidence of proximal obstruction in the EM guidance group (25%) compared with the standard technique group (22%). There was significantly improved catheter positioning in the EM guidance group, although this had no impact on shunt survival. Patients in the EM guidance group were more likely to have small or difficult-to-navigate ventricular anatomy.
Excluded Articles
Seven articles were identified, reviewed, and ultimately excluded because of weak evidence, incomplete evidence, or irrelevance regarding the application of technical adjuvants.9-15 Lam and colleagues12 discussed a Seldinger technique for placing ventricular catheters over endoscopes, and included only a single case. A paper by Chernov et al16 was excluded for a number of factors, including the fact that there were only 4 patients in one group (endoscopic third ventriculostomy [ETV]) and the inclusion range of 5–21 years included 5 patients who were 20 years of age or older.9 In a retrospective review, Shim and colleagues15 compared infants treated with ETV and shunts with infants treated with shunts alone. The authors found improved longevity of the shunt when combined with ETV. Gil et al11 retrospectively evaluated ventricular catheter placement with a frameless optical navigation system, but their study included only 9 patients and was excluded for having a sample size smaller than 10. McMillen et al13 used EM image guidance for a variety of conditions in children that included only 3 cases of hydrocephalus. Piatt and Garton’s paper14 was excluded because it was an analysis of shunt failure and related infection symptoms and frequencies using data derived from two large multicenter studies without direct reference to the techniques being considered in this review. Finally, Farahmand and colleagues10 presented information on a large group of patients older than 16 years of age without separately reporting individuals between the ages of 16 and 19 years, who could have been included.
2020 Update
This review yielded 118 abstracts, of which 8 were selected for full text review. Seven studies were excluded after review8,17-22. There were 4 studies17,18, relevant to ultrasound, but only Whitehead et al23 met inclusion criteria. This study is based on class II data indicating that ultrasound assisted shunt catheter placement did not result in a statistically significant improvement in shunt survival. Studies relevant to endoscopy19 and image guidance20,21 did not meet criteria for inclusion. In conclusion, Whitehead et al23 confirmed the recommendation from the original guideline that ultrasound is an option.
Conclusions
Endoscopy
Recommendation: There is insufficient evidence to recommend using endoscopic guidance for routine ventricular catheter placement. Strength of Recommendation: Level I, high degree of clinical certainty.
Ultrasound Guidance
Recommendation: The routine use of ultrasound-assisted catheter placement is an option. Strength of Recommendation: Level III, unclear clinical certainty.
Electromagnetic Image Guidance
Recommendation: The routine use of computer assisted electromagnetic (EM) navigation is an option. Strength of Recommendation: Level III, unclear clinical certainty.
The availability and quality of evidence is variable throughout the literature for the application of technical adjuvants for catheter placement in the treatment of hydrocephalus by CSF shunting. The strongest body of evidence applies to the use of endoscopy in insertion of shunts. Based on this evidence, endoscopy cannot be recommended for routine use, as no benefit of its application could be identified in the available literature. Less evidence exists for ultrasound and EM image guidance, and therefore a conclusive recommendation cannot be made. Catheter position may be optimized with the application of these technologies, although they may not have an impact on overall outcome with regard to shunt longevity. Insufficient data exist for the use of technical adjuncts in patients with more challenging anatomy, or in the situation in which the ventricle is unable to be cannulated using standard anatomical techniques.
Acknowledgments
We acknowledge the American Association of Neurological Surgeons (AANS)/Congress of Neurological Surgeons (CNS) Joint Guidelines Committee for the members’ reviews, comments, and suggestions; Laura Mitchell, Guidelines Project Manager for the CNS, for her contributions; Pamela Shaw, research librarian, for her assistance with the literature searches; Kevin Boyer for his assistance with data analysis; and Sue Ann Kawecki for her assistance with editing. We also acknowledge the following peer reviewers for their contributions to review the update to the guidelines: Jennifer Sweet, MD, Brandon Rocque, MD, Christoph Greissenauer, MD, Jeffrey Olson, MD.
Disclosure
The systematic review and evidence-based guidelines were funded exclusively by the CNS and AANS Pediatric Section, which received no funding from outside commercial sources to support the development of this document.
Conflict(s) of Interest: None. All Task Force members declared any potential conflicts of interest prior to beginning work on this evidence review.
Conflict(s) of Interest: None. All Pediatric Hydrocephalus Systematic Review and Evidence-Based Guidelines Update Task Force members declared any potential conflicts of interest prior to beginning work on this systematic review and evidence-based guidelines.
Author contributions to the study and manuscript preparation include the following. Conception and design: AANS/CNS Joint Section on Pediatrics. Acquisition of data: all authors. Analysis and interpretation of data: all authors. Drafting the article: Flannery. Critically revising the article: all authors. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: Flannery. Administrative/technical/material support: all authors. Study supervision: Flannery.
References
- Vries JK. Endoscopy as an adjunct to shunting for hydrocephalus. Surg Neurol. 1980;13(1):69-72.
- Kellnar S, Boehm R, Ring E. Ventriculoscopy-aided implantation of ventricular shunts in patients with hydrocephalus. Journal of pediatric surgery. 1995;30(10):1450-1451.
- Villavicencio AT, Leveque JC, McGirt MJ, Hopkins JS, Fuchs HE, George TM. Comparison of revision rates following endoscopically versus nonendoscopically placed ventricular shunt catheters. Surg Neurol. 2003;59(5):375-379; discussion 379-380.
- Kestle JR. Administrative database research. Journal of neurosurgery. 2015;122(2):441-442.
- Whitehead WE, Jea A, Vachhrajani S, Kulkarni AV, Drake JM. Accurate placement of cerebrospinal fluid shunt ventricular catheters with real-time ultrasound guidance in older children without patent fontanelles. Journal of neurosurgery. 2007;107(5 Suppl):406-410.
- Clark S, Sangra M, Hayhurst C, et al. The use of noninvasive electromagnetic neuronavigation for slit ventricle syndrome and complex hydrocephalus in a pediatric population. Journal of neurosurgery Pediatrics. 2008;2(6):430-434.
- Hayhurst C, Beems T, Jenkinson MD, et al. Effect of electromagnetic-navigated shunt placement on failure rates: a prospective multicenter study. Journal of neurosurgery. 2010;113(6):1273-1278.
- Levitt MR, O'Neill BR, Ishak GE, et al. Image-guided cerebrospinal fluid shunting in children: catheter accuracy and shunt survival. Journal of neurosurgery Pediatrics. 2012;10(2):112-117.
- Chernov MF, Kamikawa S, Yamane F, Ishihara S, Hori T. Neurofiberscope-guided management of slit-ventricle syndrome due to shunt placement. Journal of neurosurgery. 2005;102(3 Suppl):260-267.
- Farahmand D, Hilmarsson H, Hogfeldt M, Tisell M. Perioperative risk factors for short term shunt revisions in adult hydrocephalus patients. Journal of neurology, neurosurgery, and psychiatry. 2009;80(11):1248-1253.
- Gil Z, Siomin V, Beni-Adani L, Sira B, Constantini S. Ventricular catheter placement in children with hydrocephalus and small ventricles: the use of a frameless neuronavigation system. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2002;18(1-2):26-29.
- Lam S, Harris DA, Lin Y, Rocque BG, Ham S, Pan IW. Outcomes of endoscopic third ventriculostomy in adults. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2016;31:166-171.
- McMillen JL, Vonau M, Wood MJ. Pinless frameless electromagnetic image-guided neuroendoscopy in children. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2010;26(7):871-878.
- Piatt JH, Garton HJ. Clinical diagnosis of ventriculoperitoneal shunt failure among children with hydrocephalus. Pediatric emergency care. 2008(4):201-210. http://www.mrw.interscience.wiley.com/cochrane/clcentral/articles/377/CN-00631377/frame.html.
- Shim KW, Kim DS, Choi JU. Simultaneous endoscopic third ventriculostomy and ventriculoperitoneal shunt for infantile hydrocephalus. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2008;24(4):443-451.
- !!! INVALID CITATION !!! {}.
- Heussinger N, Eyupoglu IY, Ganslandt O, Finzel S, Trollmann R, Jungert J. Ultrasound-guided neuronavigation improves safety of ventricular catheter insertion in preterm infants. Brain & development. 2013;35(10):905-911.
- Crowley RW, Dumont AS, Asthagiri AR, et al. Intraoperative ultrasound guidance for the placement of permanent ventricular cerebrospinal fluid shunt catheters: a single-center historical cohort study. World neurosurgery. 2014;81(2):397-403.
- Beez T, Sarikaya-Seiwert S, Steiger HJ, Hanggi D. Real-time ultrasound guidance for ventricular catheter placement in pediatric cerebrospinal fluid shunts. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2015;31(2):235-241.
- Roth J, Constantini S. Selective use of intra-catheter endoscopic-assisted ventricular catheter placement: indications and outcome. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2012;28(8):1163-1169.
- Hermann EJ, Capelle HH, Tschan CA, Krauss JK. Electromagnetic-guided neuronavigation for safe placement of intraventricular catheters in pediatric neurosurgery. Journal of neurosurgery Pediatrics. 2012;10(4):327-333.
- Thomale UW, Knitter T, Schaumann A, et al. Smartphone-assisted guide for the placement of ventricular catheters. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2013;29(1):131-139.
- Whitehead WE, Riva-Cambrin J, Wellons JC, 3rd, et al. No significant improvement in the rate of accurate ventricular catheter location using ultrasound-guided CSF shunt insertion: a prospective, controlled study by the Hydrocephalus Clinical Research Network. Journal of neurosurgery Pediatrics. 2013;12(6):565-574.